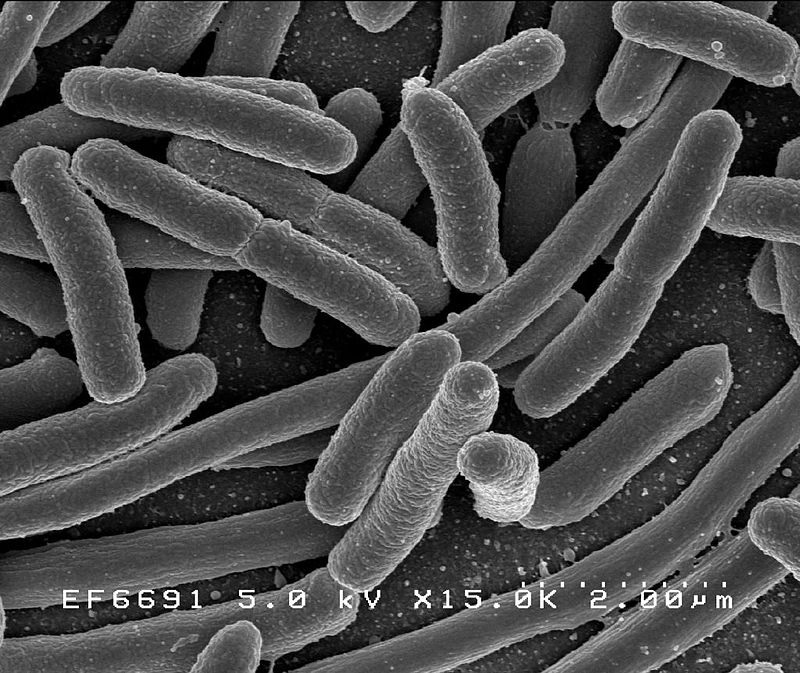
A brand new study in JAMA Psychiatry adds to the growing list of research showing what a dramatic role gut bacteria might play in our mental health.
Specifically, this study found that those with depression, anxiety, bipolar disorder, and psychosis were more likely to have lower levels of the anti-inflammatory bacteria, faecalibacterium and coprococcus.
Meanwhile, they had higher levels of of the pro-inflammatory bacteria, Eggerthella.
The study’s first author, Viktoriya Nikolova, concluded, “we have found that there is a significant overlap between gut health and the prevalence of mental illness, specifically in relation to the predominance of certain proinflammatory bacteria compared to anti-inflammatory bacteria.”
Pretty amazing huh?
Now of course, our gut bacteria is influenced by what we eat, but this doesn’t solve the chicken-egg problem.
Are people with depression etc more likely to eat food that contributes to a poor gut microbiome? Are they more likely to go sleepless? To feel stress? All of those things can affect our gut microbiome.*
In other words, does the mental health disorder precede the development of bad gut health, or can “gut dysbiosis” actually contribute to the development of mental health disorders?
The answer is probably complicated, but theoretically, it seems the gut dysbiosis found in the article could, indeed, contribute to the development of new mental health disorders.
That’s because chronic-low grade inflammation has been linked to all kinds of mental health disorders, and thanks to the close relationship between the gut and the brain, what happens in the gut often doesn’t stay in the gut. And what happens in the brain often doesn’t stay in the brain.
There’s a bidirectionality to it.
Or as a 2019 study in Clinical and Experimental Immunology put it: “Rather than being distinct systems, there is compelling evidence for bidirectional communication between gut and brain, driven by neural, metabolic, endocrine and inflammatory mediators. An emerging concept is that depressive symptoms may be mechanistically linked to excess inflammation and dysregulation of the gut–brain axis.”
Now there are a few things to remember.
There’s a field of research and thought called “nutritional psychiatry” that is much more complicated than “you are what you eat” but is still largely based on something like “you are a lot of what you eat.”
Writing in Harvard Health, Dr. Eva Selhub notes:
*****************************************************************************************************************************
“Studies have compared “traditional” diets, like the Mediterranean diet and the traditional Japanese diet, to a typical “Western” diet and have shown that the risk of depression is 25% to 35% lower in those who eat a traditional diet. Scientists account for this difference because these traditional diets tend to be high in vegetables, fruits, unprocessed grains, and fish and seafood, and to contain only modest amounts of lean meats and dairy.
They are also void of processed and refined foods and sugars, which are staples of the “Western” dietary pattern. In addition, many of these unprocessed foods are fermented, and therefore act as natural probiotics.
This may sound implausible to you, but the notion that good bacteria not only influence what your gut digests and absorbs, but that they also affect the degree of inflammation throughout your body, as well as your mood and energy level, is gaining traction among researchers.”
*****************************************************************************************************************************
As we’ve talked about on this blog, more research is finding a link among our gut microbiome, chronic inflammation, and the development of neurodegenerative diseases.
For example, mental health disorders seem to raise the likelihood of an earlier onset of conditions like dementia and Parkinson’s, and some researchers are increasingly looking at the striking similarities between neurodegenerative diseases and depression.
But there are also tons of other things — beyond our gut microbiome — linked to our mental health. Our genetic predispositions, environment, childhood, trauma, etc., (Of course, all of those could have an effect on our microbiome but that’s another question for another day).
So, while it’s awesome to start eating in ways that reduce inflammation and promote gut health, don’t be discouraged if it doesn’t work.
There are factors playing a role far outside the realm of diet in mental health disorders.
Diet might help you. In fact, research suggests you’ve got a pretty good shot at feeling at least somewhat better on a healthier diet.
But if it doesn’t help, don’t feel discouraged that somehow your condition is beyond hope. There are lots of us who have tried healthy eating and come up, well, empty.
Nevertheless, this is a great study that shows a pretty substantial link between certain mental health outcomes and gut bacteria.
And it’s yet another wake-up call to a Christian church that is still painfully slow to acknowledge that much of the source of our mental pain comes from some medical and certainly not spiritual source.
*Here’s a good article on ways to improve your gut health.