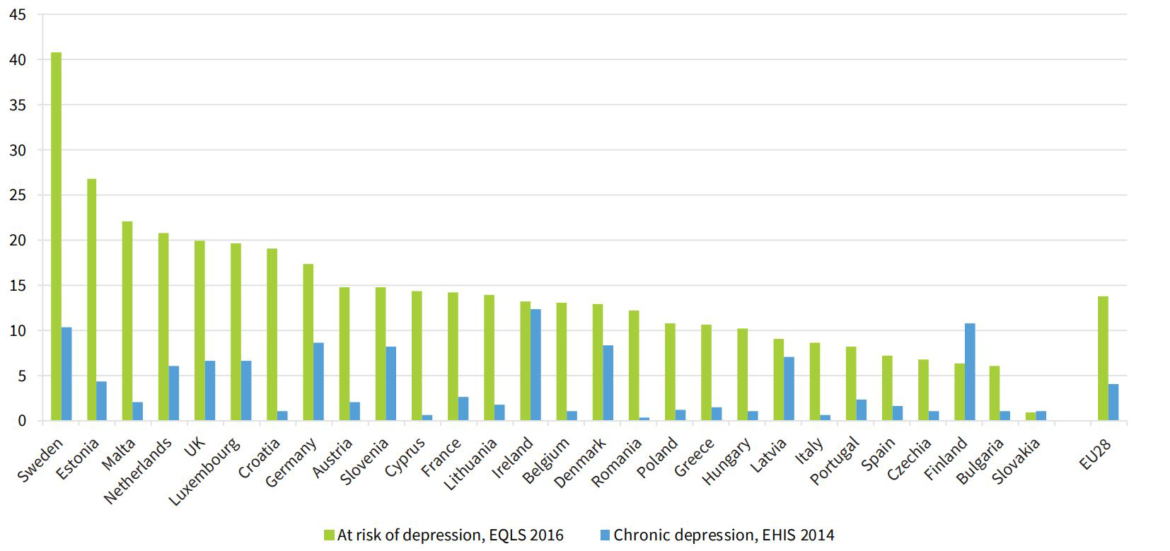
We’re used to seeing Sweden (and other Nordic countries) at the top of so many lists of best countries for XYZ. XYZ is usually something related to quality of life.
Sweden, as it turns out, is #2 on Quality of Life, #6 on Good Country List (defined as contributors to global well-being), and #7 on happiness.
That might be about to change.
A new study of EU member nations shows Swedish youth are, by far, at the highest risk for depression.
A whopping 41% of Swedes 18-24 years old are listed as risks for depression, considerably higher than runner-ups Estonia and Malta.
One possible explanation?
The report highlights widespread feelings of marginalisation among young people in Europe due to the economic crisis. Presenting in-depth case studies of support services in five Member States, it notes the significant spike in child and youth homelessness in several countries since the crisis – including in economically advanced Member States typically characterised by welfare states and higher levels of social spending.