A landmark new study in the journal Movement Disorders suggests that preexisting bipolar disorder worsens the course of Parkinson’s Disease, and is “associated with greater neuropsychiatric and cognitive problems, poorer treatment outcomes, and shorter survival.“
For at least six years, researchers compared 247 Parkinson’s patients with and without bipolar disorder.
Parkinson’s patients with bipolar were much more likely to pass away earlier, and had significantly worse neuropsychiatric symptoms that are often seen in Parkinson’s patients, including impulse control disorders, delusions, depressions, abnormal movements and behaviors.
Further, the study seemed to highlight a potential genetic component.
.”….earlier and more frequent neuropsychiatric symptoms also were associated with BSD-PD when the team looked at a subset of 34 BSD-PD and 79 PD patients carrying mutations in the GBA and PRKN genes, which have been linked to familiar Parkinson’s.”
There are some good theories on why there seems to be a relationship between bipolar and Parkinson’s. (Some research has suggested that those with bipolar are at a 3.4x greater risk of actually developing Parkinson’s later in life).
Dr. Gregory Pontone at Johns Hopkins told MedPage Today of another landmark study in 2019: “One possibility is that bipolar disorder, depression, and even anxiety — the affective illnesses — create some sort of neurological scar or damage that either opens a window for subsequent neuropathology, or erodes or dysregulates some of the same neurotransmitter pathways that make ‘fertile ground’ for neurodegenerative disorders to enter.”
This is something scientists are finding, over and over, with mental illness. An association, sometimes causative, certainly correlative, with risk for later neurodegenerative diseases.
Take depression.
A 2020 study found that people with depression were twice as likely to develop dementia later in life.
A particularly stunning result from the study was that a sibling with depression was greater than 20x more likely to develop dementia than a brother or sister or who wasn’t depressed. Amazing.

In other words, all other things equal, if Wilbur Wright were depressed and Orville wasn’t, Wilbur might have had a 20+ greater likelihood of developing dementia than his brother.
Or take anxiety.
A 2015 study found that those with “high anxiety” had a 48% higher risk of developing dementia, and the higher the anxiety, the higher the risk.
One potential mechanism: The stress hormone, cortisol. Chronically high levels “damage parts of the brain such as the hippocampus, which stores memory, and the frontal cortex, which is responsible for high-level thinking.”
There are loads of studies like these, linking mental health in younger age to neurodegenerative conditions in older age, and I’m not trying to be a bummer and further depress you by posting them!
But there are two reasons I highlight them.
First, it should motivate younger and middle-aged folks who think they’ve got plenty of time to treat their mental health….. to do it now.
I know motivation is hard to come by when you’re depressed (and there’s a scientific reason for that), and when you’re depressed, you really don’t care about your health. In fact, you often have a death wish. Even if it’s not an active death wish, you’re still lying with your eyes shut and a blanket over your head and barely breathing. Kind of like death.
So I know it’s hard to take action when you don’t care.
But please talk to a doctor about treatment. It might brighten your life and the lives of those around you, and could help lower your risk of dementia, later in life, too.
Think of it as the story of Joseph and the Egyptian famine.
There were seven feast and famine years, and Joseph famously prepped for the famine by making arrangements during the feast years.
As folks who battle mental health, we have our feast and famine times, too, and we need to be like Joseph during the feast, and start preparing for the coming famine.
I screw this up all the time.
When I’m feeling well, I think I’ve turned a corner and have hit the open road to mental health freedom. Roll down the window and see the world. But then, soon enough and inexplicably, I find myself trapped again. The open road was just a circle, leading right back to the trap.
This is unbelievably common for those struggling with mental health. The remission and relapse.
And it’s because we forget about prepping for the famine during the feast.
The second reason I post the study is that it’s further confirmation of the link between our mental and physical health. The mental is physical.
And for us Jesus-followers, one of the most comforting and profound revelations is that our depression and anxiety aren’t defects of spirituality or faith.
Unfortunately, a lot of Christians still blame defective spirituality for their mental health, and more tragically, are beaten up by spiritual leaders who claim we’re faithless or cultivating some hidden sin.
So what’s why I spend a lot of time on the Health News section of this blog.
Not just for educational purposes, but also to remind us that we’re dealing more with genetics, gut bacteria and inflammation than spiritual deficits.
And also, hopefully, to prompt us into getting treatment. Both for now and later.
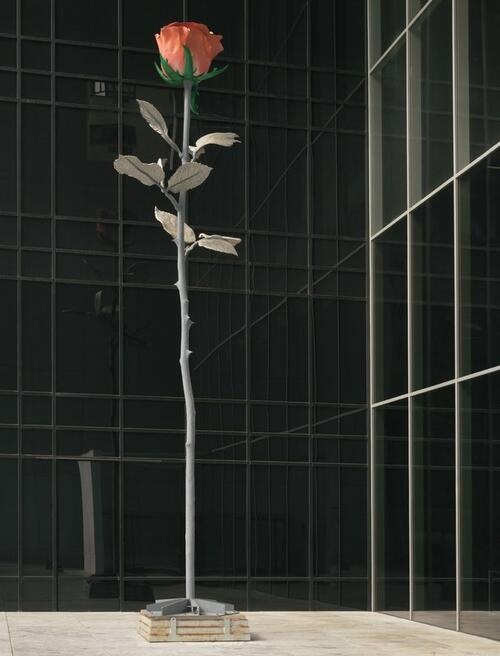
[Painting: Rose II by Isa Genzken, an artist who’s spoken of her bipolar disorder. She has an amazing story, and has produced great beauty despite her great pain. Read here for other artists who’ve struggled with the disorder]